Curtis Jackson was living his dream life — a loving and supportive wife, three wonderful kids, and a future that looked as bright as could be.
Then, one day, without warning, the dream was shattered.
At only 46, Curtis was diagnosed with cholangiocarcinoma, one of the deadliest and most aggressive forms of cancer. It’s a silent killer that strikes the liver. It is often diagnosed in later stages, leaving patients with few treatment options and little time to live.
The Jackson family turned to Mayo Clinic, where a team of experts fought the cancer with a weapon rarely used in the battle against this aggressive form of cancer.
Watch: A rare cancer. A rare weapon. Curtis Jackson’s inspiring story of survival.
Journalists: Broadcast-quality video (2:17) is in the downloads at the end of this post. Please courtesy: “Mayo Clinic News Network.” Read the script.
The rare cancer
Years before his cancer diagnosis, Curtis was diagnosed with primary sclerosing cholangitis (PSC). PSC is a chronic liver disease that causes inflammation and scarring to the bile ducts, which work with the liver to help with digestion.
PSC put the Arizona man at higher risk for liver cancer, requiring him to get regular diagnostic screenings. As with most forms of cancer, but particularly cholangiocarcinoma, doctors say early detection is key to improving patient outcomes.
However, with cholangiocarcinoma, there are often no warning signs or symptoms alerting patients of the need to consult with their doctor about getting screened, until it’s too late. In Curtis’ case, the cholangiocarcinoma was detected in one of his routine screenings at Mayo Clinic, which doctors say likely helped save his life.

“It’s a very rare cancer that tends to grow unnoticed,” says Dr. Tanios Bekaii-Saab, an oncologist with the Mayo Clinic Comprehensive Cancer Center in Arizona. “If the cancer gets to the point where it’s too advanced for surgery or transplantation, universally this is a noncurative or noncurable cancer.”
The rare weapon
Doctors say a liver transplant can sometimes be an option for some patients. However, not many transplant centers perform liver transplants on patients diagnosed with cholangiocarcinoma. Mayo Clinic is one of the few centers that do offer liver transplantation for some patients who meet certain criteria.
In Curtis’ case, doctors at Mayo Clinic determined a liver transplant was his best chance for survival.
“We’re not just here treating the cancer. We’re also treating the disease that led to the cancer.”
Dr. Tanios Bekaii-Saab, Mayo Clinic Comprehensive Cancer Center in Arizona
“It is a unique form of therapy that is based on research that started at Mayo Clinic in Rochester, Minnesota,” says Dr. Aqel Bashar, director of the Mayo Clinic Transplant Center in Arizona.
“We developed some protocols that helped us improve the outcome of transplant in these patients, and without these protocols, a lot of patients with this type of cancer would not make it to transplant,” says Dr. Aqel.
“Mayo Clinic’s ability to offer this curative option for rare cancers like this has differentiated us from many other transplant centers.”
Dr. Bashar Aqel, Director, Mayo Clinic Transplant Center in Arizona
The treatment
Curtis first underwent chemotherapy and radiation at Mayo Clinic. He was then placed on the liver transplant waiting list for a donor organ. While waiting, Curtis says he kept his focus on his family.
“I spent all the time I could with my wife and kids, like basketball practices, homework, anything we could do to help our kids,” says Curtis.
When Curtis got the call a donor organ was found, he immediately reported to Mayo Clinic to undergo his lifesaving liver transplant. The surgery was a success. Four weeks later, Curtis was back at home with family recovering well and feeling a deep sense of gratitude for his organ donor and his team at Mayo Clinic.

“Thank you because now I get to see my daughters get married, go to college, I get to see my son live his dreams and go to college and get married,” says Curtis. “I get to live and grow old with my wife. I can’t say this enough to everyone, ‘thank you.'”
“What Mayo has done to make these transplants happen is a miracle.”
Curtis Jackson, liver transplant recipient and cancer survivor
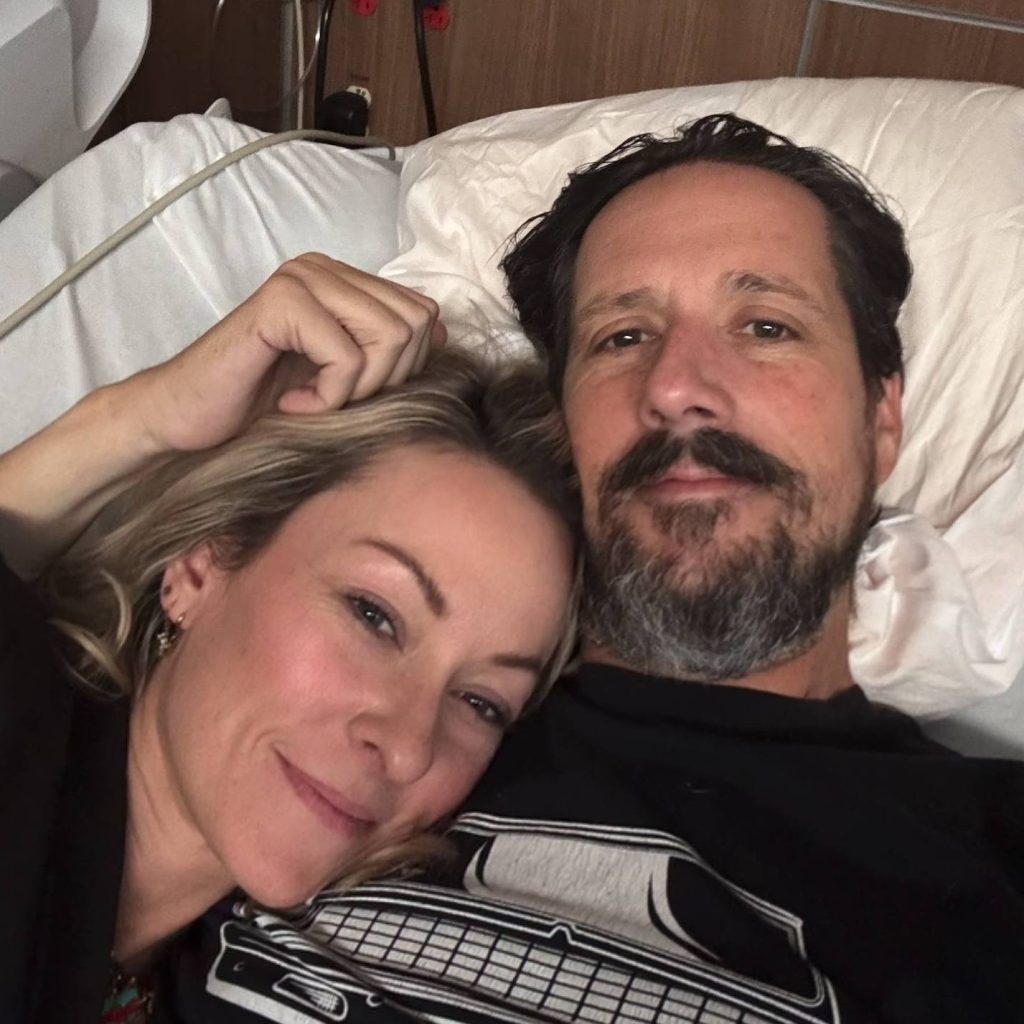
“We are already seeing signs that his new liver is functioning extremely well, and most of his liver tests have come back normal,” says Dr. Aqel. “It is an impressive recovery in a short amount of time.”
“A lot of love goes out to the people in that family,” says Gwyn, Curtis’ oldest daughter in reference to the organ donor’s family. “They allowed us to have our dad back and we’re so grateful because we love him so much.”
Doctors at Mayo Clinic are monitoring Curtis’ progress closely. Meanwhile, Curtis’ future is back to looking bright, only now with even deeper gratitude in his heart.
“This truly is the gift of life,” says Curtis.
Related stories:
- (VIDEO) Breathing easy thanks to the gift of life and new Mayo Clinic Lung Transplant Program in Arizona
- Breaking barriers: Helping Native Americans in need get the gift of life
- Jessie’s Journey
- (VIDEO) Harnessing the power of innovation and a patient’s will to survive
The post (VIDEO) A rare cancer. A rare weapon. Curtis Jackson’s inspiring story of survival appeared first on Mayo Clinic News Network.