Changes in how brain cells generate energy may drive the development of Alzheimer’s disease and influence how patients respond to therapy, according to a new study from Mayo Clinic researchers. The findings, published in the journal Alzheimer’s & Dementia, spotlight mitochondrial complex I — a critical component of cellular energy production — as both a contributor to disease progression and a promising target for new treatments.
Led by senior author Eugenia Trushina, Ph.D., the Mayo Clinic team found that disruptions in complex I activity can trigger gene expression patterns commonly observed in Alzheimer’s disease. The researchers demonstrated that using small molecules to gently adjust how complex I functions can help activate protective mechanisms in brain cells.
“This research offers new clues about how Alzheimer’s begins and shows a promising new path for developing better, more personalized treatments,” says Dr. Trushina, a researcher who studies neurodegenerative diseases.
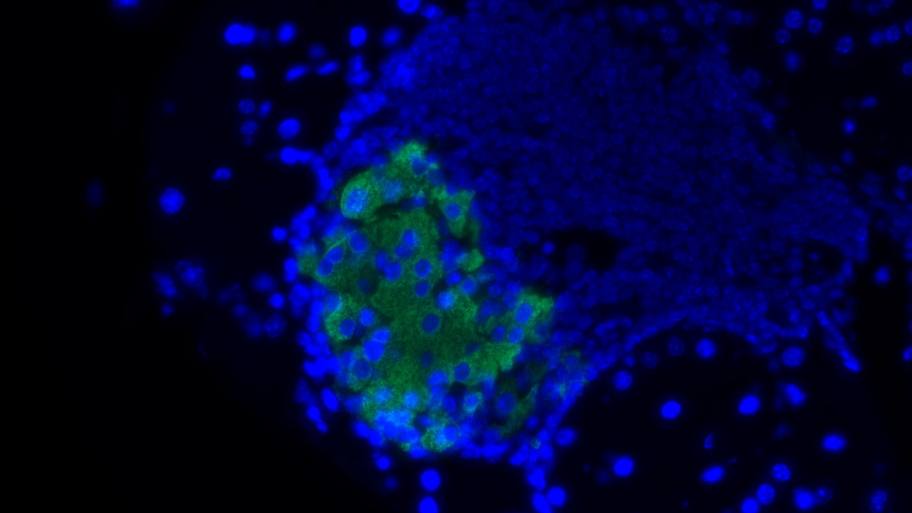
Mitochondria, often described as the powerhouse of the cell, produces the energy necessary for proper cellular function. In neurons, which have especially high energy demands, mitochondrial dysfunction can have devastating consequences. The Mayo Clinic researchers found that when complex I is not working properly, it disrupts how brain cells manage energy and respond to stress — changes that resemble those seen in the brains of people with Alzheimer’s disease.
Using experimental models and advanced molecular and computational tools, the team showed that mild modulation of complex I activity with specially designed small molecules helped neurons launch protective responses, such as reducing inflammation and improving energy balance.
Interestingly, they found that males and females responded differently to these treatments, suggesting a need for sex-specific approaches to therapy. “This sex-dependent effect is intriguing,” says Dr. Trushina. “It suggests that future therapies could be tailored by sex, especially for a disease like Alzheimer’s that affects men and women differently.”
Current Alzheimer’s treatments mostly focus on managing symptoms or targeting hallmark brain changes such as amyloid plaques and tau tangles. However, these approaches have seen limited success in halting disease progression. The new study points to mitochondrial dysfunction as a possible upstream trigger — one that may begin long before cognitive symptoms emerge.
“This study gives us a deeper understanding of the cellular events that spark Alzheimer’s and, more importantly, how we might intervene to slow or prevent its progression,” says Dr. Trushina. “Our results open the door to a new class of drugs that work by protecting the brain’s energy supply and buffering it against early disease-related changes.”
The research is part of a larger effort at Mayo Clinic called the Precure initiative, focused on developing tools that empower clinicians to predict and intercept biological processes before they evolve into disease or progress into complex, hard-to-treat conditions. In the future, the team plans to further investigate the safety and effectiveness of complex I modulators in preclinical models, with the goal of advancing into clinical trials.
The post Mitochondrial dysfunction linked to Alzheimer’s onset and treatment response appeared first on Mayo Clinic News Network.